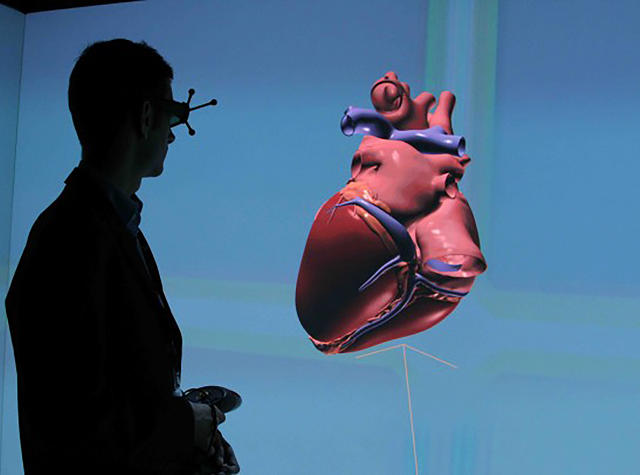
I stand, a cyborg micronaut, in front of the biggest human heart any person has ever seen.
It is Arch Obler huge, a flesh pump the size of a skyscraper, but I manipulate it with god-like facility, rotating it in midair with my hands and bisecting it with just a flick of the finger. Through ventricles and thundering aorta I dive, floating through heart chambers so enormous, they become corpuscle cathedrals.
From all sides, I am swallowed by this living, beating heart, but I am not in danger. By just thumbing a button at my fingertips, I could easily shrink it down to the size of my hand, or make it disappear entirely.
But this is just a preview of things to come. Because I've been told that in a few years, it won't be any heart I swim through. It will be a digital twin of my own.
The Living Heart Project
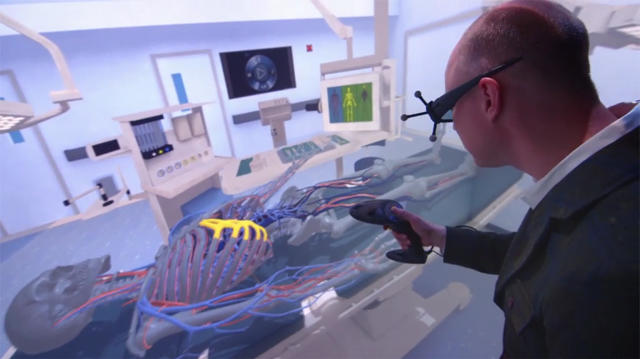
When I take off my goggles, I'm not standing in a human heart anymore. I'm standing in a multimillion-dollar virtual reality "cave" off I-95 in the Waltham, Massachusetts, headquarters of Dassault Systèmes.
Dassault is a 3-D software design company you probably never have heard of. The company sells powerful 3-D simulation systems to companies like Tesla that lets it, for example, crash test its latest car designs in virtual reality, no dummies required. Another client is Boeing, which uses Dassault's software to design and test plane parts virtually. The benefits are that new parts and designs can be tested without building—or destroying—physical models.
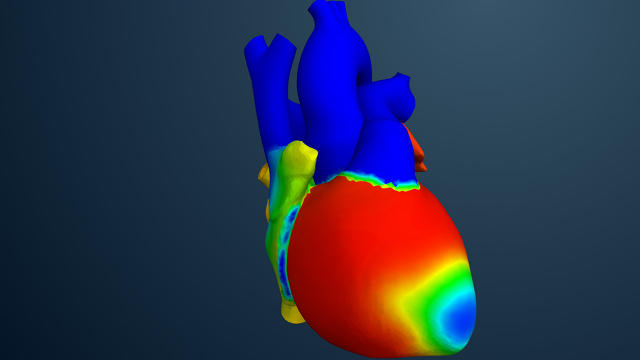
With the Living Heart Project, or LHP, Dassault is trying to bring this same technology to medicine. It simulates—in VR, or on a 3-D kiosk somewhat similar to a big Nintendo 3DS—a baseline healthy human heart, which can then be used to study things like congenital heart disease or heart defects, or how foreign bodies like medical implants or new drugs interact with it.
And that's just the start. Imagine a future in which a doctor can see what's happening in your heart by strapping on an Oculus Rift and going inside it; one in which medical students can practice on virtual patients exhibiting rare conditions they might never see in a training hospital; one where new drugs and risky new surgical techniques can be tested virtually again and again, before they are ever tried on a physical heart.

Simulating A One-In-A-Million Heart
The Living Heart Project is the personal project of Steve Levine, senior director of Dassault's SIMULA division. A material scientist by training, Levine doesn't have a medical background. But what he does have is a daughter with a congenital heart deficiency.
Jesse Levine, 26, was born with a congenital heart condition in which her primary arteries and ventricles are transposed. This means that the wrong pumps and valves are responsible for keeping blood flowing properly through her body. Because her electrical system is disrupted, she had her first pacemaker installed when she was two; she has had three replacements since then.
The Living Heart Project was born out of Levine's frustration with the fact that no one seemed to understand how his daughter's heart worked on a fundamental level. "So much of medicine is learning by direct observation," Levine says. "That's great for people like you and me, because there are millions of us. But for people like my daughter? Her condition makes her one in a million."
So Levine set out to build a platform that would eventually allow him to understand his daughter's heart as a material scientist. The Living Heart Project is the result.
Creating A Digital Twin Of Any Patient's Heart
Right now, the Living Heart Project can't simulate exactly what's going on in Jesse's heart. Leveraging data from the Food and Drug Administration (FDA), the Mayo Clinic, and other partners, Dassault's software only simulates a "normal" heart. That's a necessary starting point, says Levine. From a mechanical engineering perspective, it's important to prove that your model can accurately simulate the baseline, before you start throwing it curve balls.
But even a "baseline" simulated heart can be useful in testing new types of implants and medicines and proving they work, which is why the FDA is so keenly interested. They've signed a five-year research agreement with Dassault to use the LHP to simulate the reliability of pacemaker leads, the wires that deliver an electrical system to a patient's heart. If the FDA embraces the LHP, it could speed up the time it takes to bring new medical advances to market.
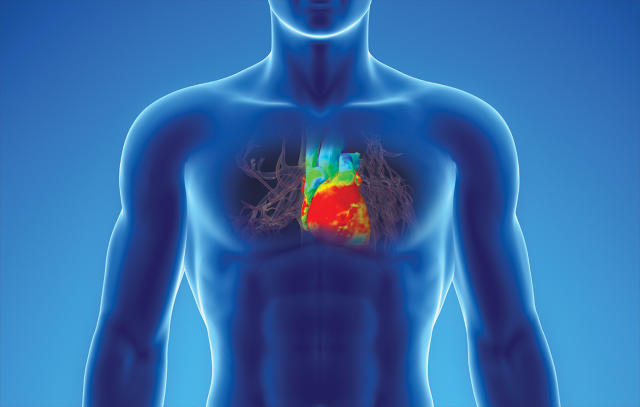
Eventually, Dassault sees the Living Heart Project evolving so that doctors will be able to simulate anyone's heart conditions in virtual reality, just by feeding it MRI data and putting on a VR headset. People with unique heart conditions like Jesse Levine will experience a better quality of care, because doctors will actually be able to explore what Dassault calls a "digital twin" her heart to custom-tailor new treatments to her unique needs.
And needless to say, if Dassault can pull off this level of medically accurate simulation, the heart's just one project. Other organs and systems such as the brain and lungs could also be simulated, until the "H" in LHP stands for "human," not "heart."
Will VR Be For Medicine What CAD Was For Architects?
That's still far off. Right now, Levine admits that even as just a heart simulator, LHP has about a decade to go before it can function as a "digital twin" of any patient's real heart. Dassault has just started, for example, working out how to simulate disease states. After that, there will be significant hurdles to getting the LHP accepted by regulatory bodies, which are still learning how to interpret data from virtual testing. Dassault also needs to convince doctors and hospitals that patient outcomes will be better if they use their software, which can only be proven after they've already done so. "It's a bit of a chicken-egg problem," admits Levine.
There's no doubt in Levine's mind, though, that software like the Living Heart Project—and, by extension, virtual reality as a whole—is going to eventually make a big impact on the medical industry.
"Our minds are built to work in 3-D, but for years, doctors have had to make do with trying to understand the body through one- and two-dimensional data sets," he says. When affordable virtual reality systems like the Oculus Rift reach a tipping point, Levine likens the transition doctors will make to what happened when architects were able to make the leap from pencil drawings to CAD programs. Doctors will finally be able to achieve a "fundamental understanding" of how a patient's body works through simulation and direct observation, allowing them to give better treatment, save lives, and reduce the cost of health care over time.
"I would say that VR is unequivocally the future of medicine," Levine says. "It's just a question of when."
All Images: via Dassault Systèmes